Sample Answer for NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders Included After Question
In this exercise, you will complete a 5-essay type question Knowledge Check to gauge your understanding of this module’s content.
Possible topics covered in this Knowledge Check include:
- Stroke
- Multiple sclerosis
- Transient Ischemic Attack
- Myasthenia gravis
- Headache
- Seizure disorders
- Head injury
- Spinal cord injury
- Inflammatory diseases of the musculoskeletal system
- Osteoporosis
- Osteopenia
- Bursitis
- Tendinitis
- Gout
- Lyme Disease
- Spondylosis
- Fractures
- Parkinson’s
- Alzheimer’s
Three basic bone-formations:
- Osteoblasts
- Osteocytes
- Osteoclasts
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
BY DAY 7 OF WEEK 7
Complete the Knowledge Check by Day 7 of Week 7.
A Sample Answer For the Assignment: NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders
Title: NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders
Scenario 1: GoutA 68-year-old obese male presents to the clinic with a 3-day history of fever with chills, and Lt. great toe pain that has gotten progressively worse. Patient states this is the first time that this has happened, and nothing has made it better and walking on his right foot makes it worse. He has tried acetaminophen, but it did not help. He took several ibuprofen tablets last night which did give him a bit of relief. HPI: hypertension treated with Lisinopril/HCTZ . SH: Denies smoking. Drinking: “a fair amount of red wine” every week. General appearance: Ill appearing male who sits with his right foot elevated. PE: remarkable for a temp of 100.2, pulse 106, respirations 20 and BP 158/92. Right great toe (first metatarsal phalangeal [MTP]) noticeably swollen and red. Unable to palpate to assess range of motion due to extreme pain. CBC and Complete metabolic profile revealed WBC 15,000 mm3 and uric acid 9.0 mg/dl. Diagnoses the patient with acute gout. Question:Explain the pathophysiology of gout. |
|||||||||
|
· Question 2
Click here to ORDER an A++ paper from our Verified MASTERS and DOCTORATE WRITERS: NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders
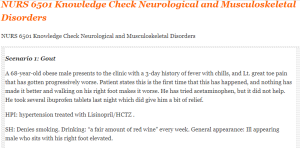
Scenario 1: Gout
A 68-year-old obese male presents to the clinic with a 3-day history of fever with chills, and Lt. great toe pain that has gotten progressively worse. Patient states this is the first time that this has happened, and nothing has made it better and walking on his right foot makes it worse. He has tried acetaminophen, but it did not help. He took several ibuprofen tablets last night which did give him a bit of relief.
HPI: hypertension treated with Lisinopril/HCTZ .
SH: Denies smoking. Drinking: “a fair amount of red wine” every week. General appearance: Ill appearing male who sits with his right foot elevated.
PE: remarkable for a temp of 100.2, pulse 106, respirations 20 and BP 158/92. Right great toe (first metatarsal phalangeal [MTP]) noticeably swollen and red. Unable to palpate to assess range of motion due to extreme pain. CBC and Complete metabolic profile revealed WBC 15,000 mm3 and uric acid 9.0 mg/dl.
Diagnoses the patient with acute gout. Question:Explain why a patient with gout is more likely to develop renal calculi. |
|||||||||
|
|||||||||
A Sample Answer 2 For the Assignment: NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders
Title: NURS 6501 Knowledge Check Neurological and Musculoskeletal Disorders
It is no coincidence that the neurological system and the musculoskeletal system share both anatomical, physiological, and functional connectivity. This structure-function relationship between the neuronal and muscular topology is responsible for influencing the disease process, the pathogenesis, presentation, diagnostic formulation, and treatment of both systems. Therefore, an understanding of the symptoms of alterations in neurological and musculoskeletal systems is a critical step in diagnosis and treatment and helps in educating the affected patients. This paper provides an account of the interplay between the neurological and the musculoskeletal system, how the racial and ethnic variables impact the physiological functioning, and how these processes interact to affect the patient.
Pathophysiologic Processes That Would Account for The Patient Presenting These Symptoms
Conspicuously, the patient has a history of hypertension and smoking that form the basis of his clinical symptoms including left-sided weakness of both the upper and lower limbs and a mild left facial droop. These features suggest a stroke. Hypertension is a well-established cause of stroke through various mechanisms that include acceleration of the arteriosclerotic process in the cerebral arteries thus increasing the risk of stenosis, embolism, and consequently infarction. Furthermore, high intravascular pressure within the cerebral arteries leads to considerable damage to the endothelial lining and alteration of the smooth muscle function (Wajngarten & Silva, 2019). This endothelial damage and altered blood cell-endothelium interaction lead to the formation of local thrombi, ischemia, and cerebral infarction whereas smooth muscle cell degeneration leads to intracerebral hemorrhages.
Smoking on the other hand is associated with an increased risk of developing a stroke. According to Pan et al. (2019) smokers have an increased risk of overall stroke compared with nonsmokers, with a pooled odds ratio of 1.61 (95% CI: 1.34–1.93). Tobacco smoke contains a lot of chemicals that include nicotine, carbon monoxide, and cyanide among many others. These chemicals increase the risk of developing atherosclerosis, platelet aggregation, hypertension, low levels of high-density cholesterol, and high levels of low-density cholesterol. A complex and multifactorial interaction of the abovementioned factors leads to impaired vascular function resulting in both cardiovascular compromise and cerebral embolism and infarction.
Racial/Ethnic Variables That May Impact Physiological Functioning
Generally, evidence shows that a racial disparity exists in the presentation of this physiological process, affecting more blacks as compared to whites. According to a study by Howard et al. (2019), the black individuals aged between 45 and 64 years had a 3-fold increase of developing stroke as compared with the whites. Black individuals have a higher preponderance of stroke because of their high risk to develop metabolic conditions such as diabetes mellitus, hypertension, obesity, hypercholesterolemia, and smoking (Tong et al., 2021).
How These Processes Interact to Affect the Patient
Neurological and musculoskeletal processes work hand in hand. Every movement the body makes requires communication between the brain and the muscles. Consequently, a pathologic process affecting the neurological process can lead to musculoskeletal manifestations such as hemiplegia, muscle spasms, muscle atrophy, and muscle pain among others. For instance, chronic musculoskeletal pain is principally considered a nervous system disorder as a result of nervous system plasticity (George & Bishop, 2018). Similarly, several factors such as smoking, hypertension, aging, and racial variables impact these physiologic systems resulting in an inherent complexity of interactions that affect patient functioning.
Conclusion
Musculoskeletal and neurological systems are correlated. Nurses must assess both systems at a given point for effective diagnosis and treatment. It is also elemental to educate the patient concerning modifiable risk factors such as smoking and hypertension that result in occurrences that limit the functioning of the musculoskeletal and neurological systems.
References
George, S. Z., & Bishop, M. D. (2018). Chronic musculoskeletal pain is a nervous system disorder… now what? Physical Therapy, 98(4), 209–213. https://doi.org/10.1093/ptj/pzy002
Howard, V. J., Madsen, T. E., Kleindorfer, D. O., Judd, S. E., Rhodes, J. D., Soliman, E. Z., Kissela, B. M., Safford, M. M., Moy, C. S., McClure, L. A., Howard, G., & Cushman, M. (2019). Sex and race differences in the association of incident ischemic stroke with risk factors. JAMA Neurology, 76(2), 179–186. https://doi.org/10.1001/jamaneurol.2018.3862
Pan, B., Jin, X., Jun, L., Qiu, S., Zheng, Q., & Pan, M. (2019). The relationship between smoking and stroke: A meta-analysis: A meta-analysis. Medicine, 98(12), e14872. https://doi.org/10.1097/MD.0000000000014872
Tong, X., Schieb, L., George, M. G., Gillespie, C., Merritt, R. K., & Yang, Q. (2021). Racial/ethnic and geographic variations in long-term survival among Medicare beneficiaries after acute ischemic stroke. Preventing Chronic Disease, 18(200242), E15. https://doi.org/10.5888/pcd18.200242
Wajngarten, M., & Silva, G. S. (2019). Hypertension and stroke: Update on treatment. European Cardiology, 14(2), 111–115. https://doi.org/10.15420/ecr.2019.11.1

