Assignment: Pediatric SOAP Note Template
Assignment Pediatric SOAP Note Template
NP Student Name: Yenixis Martinez-Castillo Child’s Initials: D.C DOB:12/30/2018
Clinical Date: 05/04/2019 Age: 4 Months Place of Born: Miami, FL
Week Soap Project: W1 Sex:
M x_
F ___ Type of Soap Note:
Well child visit __x__
Sick visit ____
SUBJECTIVE
Historian: Mother
Present Concerns/CC: “yearly exam and immunization update.”
Child Profile: Healthy appearing 4-year-old male. The mother claims the overall health status of her child is good and he is very active and playful.
Activities of Daily Living (age appropriate): He is generally a pleasant child. Feeds on a well-balanced diet and drinks plenty of water after every meal, and milk with meals. He dresses appropriately on his own but with minimal help on buttons and zips. He sleeps at night in his own bed for about 8 hours.
Safety Practices: All his baths are always supervised. The pool and hot tub are kept safe. He is normally supervised when playing outside.
Changes in daycare/school/after-school care: He is taken care of mostly by a stay at home mom.
Sports/physical activity: He plays with his toys after school, including a tennis ball.
Developmental History: He can go upstairs on his own. He can stand on one foot for about 5 seconds. He can kick a ball forward. His hand and finger skills are quite impressive as he can draw circles and squires. His language is also improving as he understands the concept of “same” and “different.” His cognitive abilities are improved as he can correctly name some colors. He is also able to socialize through playing with other children.
Sexual History (if appropriate): None
HPI: A 4-year-old normal male child, is brought to the clinic by his mother for a yearly exam and immunization update. The patient has no previous medical history or any presenting illness. He is alert, well hydrated and nourished. He seems happy and well taken care of.
Medications: None
PMH: D.C was a planned pregnancy with appropriate prenatal care. The mother was healthy during the pregnancy period and denies using tobacco, alcohol or any other illicit drugs. during pregnancy, she used medications such as daily prenatal vitamins and folic acid. She gained weight by about 35 pounds during pregnancy and delivered vaginally, without any complications. The child is very healthy with no reported infectious diseases or illness.
Allergies: NKDA
Chronic Illnesses/Major traumas: None
Hospitalizations/Surgeries: No hospitalization or surgical history reported.
Immunizations: Up to date (DTaP x 5, Hep-A x2, Hep-B x3, HIB x4, MMR x2, PCV7 x4, IPV x4, VZV x2, FLU x2)
Family Medical History: Mother and father are living healthy.
Social History: The child lives with both his parents. The mother denies using tobacco, alcohol or any illicit drugs. the mother is a stay at home mom, while the father works to earn a living for the family. The mother reports that their neighborhood is safe, and she has never been abused sexually or physically in her entire life.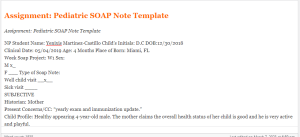
REVIEW OF SYSTEMS
General: as per the information provided by the mother, no weight changes. No chills, night sweats, fatigue or changes in energy levels. Cardiovascular: No chest tightness, chest pain, palpitations. No signs of edema or orthopnea
Skin: Normal and healthy skin with no lesions, itchiness or rashes. Respiratory: No wheezing, shortness of breath, or coughing. No history of pneumonia.
Head: Normocephalic with equal distribution of hair. Denies any physical injuries to the head.
Breast: No bumps, lumps, skin changes or nipple discharge.
Eyes: The mother denies noticing diplopia, blurry vision, changes in visual acuity or excessive tearing.
Gastrointestinal: The mother denies noticing any bloody vomits, swallowing difficulties, indigestion, nausea, hiccups, appetite loss, pain or sensation of abdominal inflation. She also denies jaundice, constipation or diarrhea.
Ears: The mother denies noticing ear discharge, earache, tinnitus or changes in hearing acuity.
Musculoskeletal: No back pain, joint stiffness, pain or swelling. No fractures.
Nose/Mouth/Throat: The mother denies noticing any dental diseases, allergies, sinus problems, nasal congestion or bleeding.
Neurological: The mother denies syncope, transient paralysis, seizure, weakness or sleeping difficulties.
Genitourinary/Gynecological: Mother denies any changes in the color of the urine, no urgency or frequency burning.
Heme/Lymph/Endo: Denies any history of blood transfusion, swollen glands, night sweats, cold or heat intolerance, increased hunger or increased thirst.
Developmental Problems: No development problems reported. Behavioral Status/Psychiatric: Very active and playful. No anxiety or depression reported.
Click here to ORDER an A++ paper from our MASTERS and DOCTORATE WRITERS: Assignment: Pediatric SOAP Note Template
OBJECTIVE
(Attach growth chart with height/weight/head circumference plotted & noting percentiles; attach these forms at the end of your SOAP note; include pertinent positives & negatives)
Weight: Temp: BP:
Height: Pulse: Respirations:
General Appearance & parent‐child interaction: The patient is well oriented in an upright position, very alert, quiet and well groomed. He is well hydrated and nourished. His interaction with the mother and medical practitioner is quite impressive.
Skin: Light, warm, clean and moist skin with no rashes or lesions.
Head: Normocephalic with equal distribution of hair, atraumatic.
Eyes: Pupils Equal and Equally Reactive to Light, intact extraocular movements, no itching or redness or any changes in visual acuity.
Ears: Intact auditory meatus with no redness or tenderness. No pain on palpitation. Passed the whisper test bilaterally.
Nose: No septal deviation. Pink nasal mucosa, well moistened.
Throat/Mouth: The tongue, lips, and mucosa with no alterations. The teeth and gums are normal. The oropharynx is pink in color without secretions.
Neck: No noted limited ROM. No occupational or cervical lymphadenopathy. No alteration of the thyroid.
Cardiovascular: Regular heart rhythms with no murmurs, rubs, gallop or clicks. Palpable Pulses 4+. The capillary refill is less than 3 seconds. No edema noted.
Respiratory: No nasal flutter noted. The chest walls are symmetric. Respiration is regular. No intercostal retractions. No dyspnea. Auscultation without alterations.
Gastrointestinal: The abdomen is soft and symmetric with no tenderness. The bowel movement is normal. No rebound or guarding. No signs of constipation or diarrhea.
Breast: There were no masses, dimples, secretions, tenderness, discoloration or wrinkling of the breasts.
Genitourinary: The external genitalia is normal with no rashes or any signs of infections.
Musculoskeletal: Full ROM noted in all the 4 extremities when the patient could move about the examination room.
Neurological: Stable balance with a normal gait. Intact mental status. The Cranial Nerves I-XII with no alterations. Normal reflexes and symmetric, normal gait, normal strength of muscles, intact sensation. A clear and normal speech tone. Stable and normal posture.
Behavioral/Psychiatric: No signs of anxiety or depression. Normal and acceptable behavior in the examination room.
Pediatric/Adolescent Assessment Tools: Denver II test: at his age, the results were normal. The Denver Developmental Screening Test II (DENVER II) is commonly used in clinical practice extensively, as it is easy to learn to implement and score and provides a structured approach in developmental assessment screening for children between 0 to 6 years old. The test is a very important tool in identifying children with developmental delay as per their age requirement (Sabanathan, Wills, & Gladstone, 2015).
Present Developmental: D.C belongs to the preschool stage of development for children between 3 to 5 years. The child is still learning the aspect of independence such as dressing by himself and walking on his own. He seems to be more assertive and takes more initiatives but is sometimes guilty as a result of being too forceful at times, just as Erikson described the basic conflict of this stage as “initiative vs. guilt” (Jones, & Russell-Fisher, 2018)
Movement: able to stand on one foot for about 5 seconds and can hop perfectly.
Hand and Finger skills: able to use age-appropriate scissors and draw several shapes.
Emotional and social skills: understand the idea of mine and his and is also friendly.
Cognitive: can correctly name familiar colors
Language: can answer simple questions and even say his name and age
Lab and/or Diagnostic Tests:
The physician uses several milestones of development to determine whether the child’s development is appropriate with his age (In McInerny, & American Academy of Pediatrics, 2017).
DIAGNOSIS
Final/Primary Diagnosis (es): Normal and healthy
PLAN:
• Return to the clinic after one year for a five-year-old well-child examination and immunization.
• Vaccines administered this visit: none
• vaccine administration forms given: none
• Medication: none
• Laboratory tests ordered: none
• Diagnostic tests ordered: none
• Non-pharmaceutical treatments: none
• Patient/Family education and Anticipatory guidance for the next well-child visit (van et al., 2015):
Communication and Language Skills: strings four or more words together to construct a sentence.
Movement and Physical Development: try to walk upstairs and downstairs with alternating feet. Try to catch a ball with both arms fully outstretched.
Social and Emotional Development: give the name of one or two of your friends. Name a game liked by your friend.
Cognitive Skills: knowing your first and last name, and your age. Take part in pretend play.
• When to Talk to see a Doctor: all children develop at their own pace, but there is a standard way in which children of a given age group are expected to grow. Report to the doctor in case your child (In McInerny, & American Academy of Pediatrics, 2017):
Is unable to speak or construct a full sentence.
has severe anxiety or depression
is unable to make strokes with a pencil or crayon
Additionally, if you notice that your child has lost some of the skills that he once had or shows weakness on one body side, inform your physician (In Hagan, In Shaw, & In Duncan, 2017).
Self-Evaluation of Interaction with patient/family during clinic visit: I am quite satisfied with the job I did in collecting both subjective and objective data for my first well-child visit for immunization update. Despite my strengths in understanding the stages of development and the different milestone, I still find it a weakness to be able to relate quite appropriately with the child to understand them even much better. I believe that with more encounters of the same, I will be able to carry out examination and assessment of pediatric patients more efficiently.
Each week, you are required to enter your patient encounters into CORE. Your faculty will be checking to ensure you are seeing the right number and mix of patients for a good learning experience. You will also need to include a minimum of one complete SOAP note using the Pediatric SOAP Note template.The SOAP note should be related to the content covered in this week, and the completed note should be submitted to the Submissions Area. When submitting your note, be sure to include the reference number from CORE.
Submission Details:
By the due date assigned enter your patient encounters into CORE and submit your Pediatric SOAP note document to the Submissions Area.
Name your SOAP note document SU_NSG6435_W3_A3_LastName_FirstInitial.doc.
Include the reference number from CORE in your document.
Additional Instructions: SOAP note should be regarding a healthy 4 year old (sex of child is irrelevant) who is presenting for a yearly exam and immunization update. anticipatory guidelines using brightfures.aap.org should be used for the parent teaching.
Lopes Write Policy
For assignments that need to be submitted to Lopes Write, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
I do not accept assignments that are two or more weeks late unless we have worked out an extension.
As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
Important information for writing discussion questions and participation
Welcome to class
Hello class and welcome to the class and I will be your instructor for this course. This is a -week course and requires a lot of time commitment, organization, and a high level of dedication. Please use the class syllabus to guide you through all the assignments required for the course. I have also attached the classroom policies to this announcement to know your expectations for this course. Please review this document carefully and ask me any questions if you do. You could email me at any time or send me a message via the “message” icon in halo if you need to contact me. I check my email regularly, so you should get a response within 24 hours. If you have not heard from me within 24 hours and need to contact me urgently, please send a follow up text to
I strongly encourage that you do not wait until the very last minute to complete your assignments. Your assignments in weeks 4 and 5 require early planning as you would need to present a teaching plan and interview a community health provider. I advise you look at the requirements for these assignments at the beginning of the course and plan accordingly. I have posted the YouTube link that explains all the class assignments in detail. It is required that you watch this 32-minute video as the assignments from week 3 through 5 require that you follow the instructions to the letter to succeed. Failure to complete these assignments according to instructions might lead to a zero. After watching the video, please schedule a one-on-one with me to discuss your topic for your project by the second week of class. Use this link to schedule a 15-minute session. Please, call me at the time of your appointment on my number. Please note that I will NOT call you.
Please, be advised I do NOT accept any assignments by email. If you are having technical issues with uploading an assignment, contact the technical department and inform me of the issue. If you have any issues that would prevent you from getting your assignments to me by the deadline, please inform me to request a possible extension. Note that working fulltime or overtime is no excuse for late assignments. There is a 5%-point deduction for every day your assignment is late. This only applies to approved extensions. Late assignments will not be accepted.
If you think you would be needing accommodations due to any reasons, please contact the appropriate department to request accommodations.
Plagiarism is highly prohibited. Please ensure you are citing your sources correctly using APA 7th edition. All assignments including discussion posts should be formatted in APA with the appropriate spacing, font, margin, and indents. Any papers not well formatted would be returned back to you, hence, I advise you review APA formatting style. I have attached a sample paper in APA format and will also post sample discussion responses in subsequent announcements.
Your initial discussion post should be a minimum of 200 words and response posts should be a minimum of 150 words. Be advised that I grade based on quality and not necessarily the number of words you post. A minimum of TWO references should be used for your initial post. For your response post, you do not need references as personal experiences would count as response posts. If you however cite anything from the literature for your response post, it is required that you cite your reference. You should include a minimum of THREE references for papers in this course. Please note that references should be no more than 5 years old except recommended as a resource for the class. Furthermore, for each discussion board question, you need ONE initial substantive response and TWO substantive responses to either your classmates or your instructor for a total of THREE responses. There are TWO discussion questions each week, hence, you need a total minimum of SIX discussion posts for each week. I usually post a discussion question each week. You could also respond to these as it would count towards your required SIX discussion posts for the week.
I understand this is a lot of information to cover in 5 weeks, however, the Bible says in Philippians 4:13 that we can do all things through Christ that strengthens us. Even in times like this, we are encouraged by God’s word that we have that ability in us to succeed with His strength. I pray that each and every one of you receives strength for this course and life generally as we navigate through this pandemic that is shaking our world today. Relax and enjoy the course!
Hi Class,
Please read through the following information on writing a Discussion question response and participation posts.
Contact me if you have any questions.
Important information on Writing a Discussion Question
- Your response needs to be a minimum of 150 words (not including your list of references)
- There needs to be at least TWO references with ONE being a peer reviewed professional journal article.
- Include in-text citations in your response
- Do not include quotes—instead summarize and paraphrase the information
- Follow APA-7th edition
- Points will be deducted if the above is not followed
Participation –replies to your classmates or instructor
- A minimum of 6 responses per week, on at least 3 days of the week.
- Each response needs at least ONE reference with citations—best if it is a peer reviewed journal article
- Each response needs to be at least 75 words in length (does not include your list of references)
- Responses need to be substantive by bringing information to the discussion or further enhance the discussion. Responses of “I agree” or “great post” does not count for the word count.
- Follow APA 7th edition
- Points will be deducted if the above is not followed
- Remember to use and follow APA-7th edition for all weekly assignments, discussion questions, and participation points.
- Here are some helpful links
- Student paper example
- Citing Sources
- The Writing Center is a great resource

