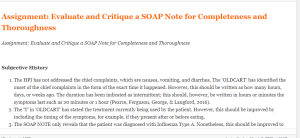
Assignment: Evaluate and Critique a SOAP Note for Completeness and Thoroughness
A Sample Answer For the Assignment: Assignment: Evaluate and Critique a SOAP Note for Completeness and Thoroughness
Title: Assignment: Evaluate and Critique a SOAP Note for Completeness and Thoroughness
Subjective History
- The HPI has not addressed the chief complaints, which are nausea, vomiting, and diarrhea. The ‘OLDCART’ has identified the onset of the chief complaints in the form of the exact time it happened. However, this should be written as how many hours, days, or weeks ago. The duration has been indicated as intermittent; this should, however, be written in hours or minutes the symptoms last such as 20 minutes or 1 hour (Pearce, Ferguson, George, & Langford, 2016).
- The ‘T’ in ‘OLDCART’ has stated the treatment currently being used by the patient. However, this should be improved by including the timing of the symptoms, for example, if they present after or before eating.
- The SOAP NOTE only reveals that the patient was diagnosed with Influenza Type A. Nonetheless, this should be improved to inform the exact time or how long ago the patient was diagnosed with the Influenza Type A.
- The medication the patient is taking was not indicated under the subjective component. Current medications should be listed to assist the health care providers in deciding which drugs should be stopped or continued in the treatment plan.
- Sexual history. The sexual history of the patient was not obtained. This should be included in the SOAP note to help in identifying whether the patient is sexually active and history of STIs (Pearce, Ferguson, George & Langford, 2016). Besides, it will facilitate patient education on safe sex education.
- Immunization history. Information on the immunization status of the patient was not obtained. The immunization history should be recorded to establish whether it is up to date as per the guidelines on immunization (Pearce, Ferguson, George & Langford, 2016). The history will further help to decide if the patient will require a booster vaccine or whether the presenting condition is as a result of lack of immunization.
- Information on known food and drug allergies has not been provided. This should be improved to include any food or drug allergies the patient has. Besides, it helps the care provider to decide which drugs to prescribe to the patient that will not result in an allergic reaction.
- Social history. The patient’s social history was included under demographics; however, this should be under the subjective history. Information on the history of cigarette smoking, alcohol consumption, and drug substance abuse should be included to help identify if the presenting symptoms are a result of substance or alcohol use (Pearce, Ferguson, George & Langford, 2016). The occupation of his parents should also be included to help establish the economic status of the family.
- In the review of the abdomen, the SOAP note indicates that the patient denies vomiting, yet the chief complaint is vomiting. The discrepancy in patient’s history should be avoided by improving the history taking technique.
Click here to ORDER an A++ paper from our MASTERS and DOCTORATE WRITERS: Assignment: Evaluate and Critique a SOAP Note for Completeness and Thoroughness
Objective History
- Vital Signs. The vital signs were recorded under the general condition, but the respiration rate was not included. To improve this, the vital signs should be recorded first in the SOAP note indicating the patient’s blood pressure, temperature, pulse, and respirations (Pearce, Ferguson, George & Langford, 2016). Recording of all vital signs helps in establishing the underlying condition and deciding the priority medical interventions that will stabilize the patient.
- Body Mass Index (BMI). The BMI was not indicated; however, it is essential that the BMI is indicated to help identify a case of overweight or underweight and offer appropriate nutrition support.
- Genito-urinary system. The system was not reviewed in objective history. This should be improved by performing a physical examination of the genitals to help identify the presence of any anomalies that could be the underlying problem.
- Neurological system. An assessment of the neurological system functioning was not conducted. This can be improved by reviewing the nerve function of both the peripheral and central nervous system.
- Arterial Blood Gas Analysis (ABGs). ABGs analysis is missing in the SOAP note objective data. The patient was experiencing shortness of breath, vomiting, and diarrhea, which could cause an alteration in the carbonic acid and bicarbonate levels in the body (Castro & Keenaghan, 2019). An ABG analysis should be conducted to facilitate in establishing if the patient has alkalosis or acidosis, which are caused by an underlying disease.
- Laboratory tests. The tests conducted included Rapid Strep test, Rapid Flu test, and Mono Spot. However, a test stool for ova and cyst test should have been undertaken to help identify the causative factor for diarrhea in the patient (Panda, Chandrakar, Bawankar & Chandi, 2016).
- Radiology tests. A radiology test, such as a chest X-ray is essential in the case of this patient to establish the cause of respiratory difficulties. Besides, it will help in coming up with a definite medical diagnosis for the patient.
Differential Diagnosis
- Acute Maxillary Sinusitis with Viral Syndrome: According to the SOAP note, this was identified as the primary diagnosis based on the patient’s history of Influenza and physical findings of maxillary sinus pain on palpation. In addition, the diagnosis was made based on fever, cough that worsened at night, nasal congestion, headache, halitosis, eye pressure, and a sore throat. The physical findings are not accurate as per the subjective data since there is no report of a cough that worsens at night. However, the positive findings on the objective data are accurate and thorough as per the physical exam.
- Streptococcal pharyngitis. The differential diagnosis was made based on the patient’s history, physical examination findings, and the negative Rapid Strep test. The criteria used to identify streptococcal pharyngitis as a possible diagnosis was not thorough. This is because the diagnosis has to have the fever, anterior cervical lymphadenopathy, exudate from the tonsillar gland, and absence of cough. The patient, however, was negative for tonsillar exudate but positive for cough.
- Infectious Mononucleosis: This was made a possible diagnosis as per the history and physical findings of fatigue, sore throat, fever, weakness, swollen tender cervical nodes, erythematous and edematous tonsils, loss of appetite and headache. A negative Mono Spot test was also used as a basis to come up with the differential diagnosis. Majority of the findings are accurate; however, the patient did not report loss of appetite.
- Adenovirus infection. This was identified as a possible diagnosis as per the patient’s history. The physical examination findings revealed sinusitis, which could be a secondary infection of Adenovirus infection and the presence of fever, cough, rhinorrhea, sore throat, diarrhea, abdominal cramps, and fatigue. Nevertheless, the positive findings for the diagnosis are not thorough since the patient did not report abdominal cramps.
- Meningitis: According to the SOAP note, the positive findings of nausea, fatigue, chills, fever, diarrhea, and myalgia made Meningitis a differential diagnosis. The patient had negative findings for tachypnea, vomiting, rash, neck stiffness, photophobia, and altered mental status that identified Meningitis as an unlikely diagnosis. Nevertheless, the data is not accurate since the patient’s subjective data did not reveal any muscle pain. The patient also had a normal range of motion and good muscle strength and coordination, which could not be achieved with myalgia. Furthermore, the patient’s chief complaint was vomiting, and this makes the negative findings stated inaccurate.
Recommendations on Health Promotion
The United States Preventative Task Force (USPTF) recommends that health care providers conduct screening for obesity in adolescents and children older than six years. Besides, it suggests that health providers should provide or refer obese children and adolescents for comprehensive and rigorous behavioral therapies that facilitate improvement in weight (Grossman et al., 2018). The USPTF further states that certain risk factors contribute to obesity, such as genetics, poor nutrition, and inadequate physical activity (Grossman et al., 2018). Poor sleep hygiene, sedentary lifestyles, and families earning a low income also significantly contribute to adolescent and child obesity.
The USPSTF recommends comprehensive and intensive behavioral approaches for a total period of 26 hours, over 2 to 12 months to facilitate weight loss (Grossman et al., 2018). Additionally, behavioral strategies for a total period of 52 hours or more resulted in a higher degree of weight loss and the prevention of cardiovascular and metabolic diseases.
Review this sample SOAP note Click for more options . Explain what needs to be done to improve this note and why. Be sure and identify the following:
Eight (8) or more data points in the subjective history that need improvement
Seven (7) or more data points in the objective history that need improvement
For each diagnosis or differential diagnosis identified, is the pertinent positive and negative data thorough and accurate?
Your response should contain a discussion of National Guidelines and ARHQ Health Promotion recommendations (according to the United States Preventative Task Force [USPTF]) appropriate to the case.
Lopes Write Policy
For assignments that need to be submitted to Lopes Write, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
I do not accept assignments that are two or more weeks late unless we have worked out an extension.
As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
Important information for writing discussion questions and participation
Welcome to class
Hello class and welcome to the class and I will be your instructor for this course. This is a -week course and requires a lot of time commitment, organization, and a high level of dedication. Please use the class syllabus to guide you through all the assignments required for the course. I have also attached the classroom policies to this announcement to know your expectations for this course. Please review this document carefully and ask me any questions if you do. You could email me at any time or send me a message via the “message” icon in halo if you need to contact me. I check my email regularly, so you should get a response within 24 hours. If you have not heard from me within 24 hours and need to contact me urgently, please send a follow up text to
I strongly encourage that you do not wait until the very last minute to complete your assignments. Your assignments in weeks 4 and 5 require early planning as you would need to present a teaching plan and interview a community health provider. I advise you look at the requirements for these assignments at the beginning of the course and plan accordingly. I have posted the YouTube link that explains all the class assignments in detail. It is required that you watch this 32-minute video as the assignments from week 3 through 5 require that you follow the instructions to the letter to succeed. Failure to complete these assignments according to instructions might lead to a zero. After watching the video, please schedule a one-on-one with me to discuss your topic for your project by the second week of class. Use this link to schedule a 15-minute session. Please, call me at the time of your appointment on my number. Please note that I will NOT call you.
Please, be advised I do NOT accept any assignments by email. If you are having technical issues with uploading an assignment, contact the technical department and inform me of the issue. If you have any issues that would prevent you from getting your assignments to me by the deadline, please inform me to request a possible extension. Note that working fulltime or overtime is no excuse for late assignments. There is a 5%-point deduction for every day your assignment is late. This only applies to approved extensions. Late assignments will not be accepted.
If you think you would be needing accommodations due to any reasons, please contact the appropriate department to request accommodations.
Plagiarism is highly prohibited. Please ensure you are citing your sources correctly using APA 7th edition. All assignments including discussion posts should be formatted in APA with the appropriate spacing, font, margin, and indents. Any papers not well formatted would be returned back to you, hence, I advise you review APA formatting style. I have attached a sample paper in APA format and will also post sample discussion responses in subsequent announcements.
Your initial discussion post should be a minimum of 200 words and response posts should be a minimum of 150 words. Be advised that I grade based on quality and not necessarily the number of words you post. A minimum of TWO references should be used for your initial post. For your response post, you do not need references as personal experiences would count as response posts. If you however cite anything from the literature for your response post, it is required that you cite your reference. You should include a minimum of THREE references for papers in this course. Please note that references should be no more than 5 years old except recommended as a resource for the class. Furthermore, for each discussion board question, you need ONE initial substantive response and TWO substantive responses to either your classmates or your instructor for a total of THREE responses. There are TWO discussion questions each week, hence, you need a total minimum of SIX discussion posts for each week. I usually post a discussion question each week. You could also respond to these as it would count towards your required SIX discussion posts for the week.
I understand this is a lot of information to cover in 5 weeks, however, the Bible says in Philippians 4:13 that we can do all things through Christ that strengthens us. Even in times like this, we are encouraged by God’s word that we have that ability in us to succeed with His strength. I pray that each and every one of you receives strength for this course and life generally as we navigate through this pandemic that is shaking our world today. Relax and enjoy the course!
Hi Class,
Please read through the following information on writing a Discussion question response and participation posts.
Contact me if you have any questions.
Important information on Writing a Discussion Question
- Your response needs to be a minimum of 150 words (not including your list of references)
- There needs to be at least TWO references with ONE being a peer reviewed professional journal article.
- Include in-text citations in your response
- Do not include quotes—instead summarize and paraphrase the information
- Follow APA-7th edition
- Points will be deducted if the above is not followed
Participation –replies to your classmates or instructor
- A minimum of 6 responses per week, on at least 3 days of the week.
- Each response needs at least ONE reference with citations—best if it is a peer reviewed journal article
- Each response needs to be at least 75 words in length (does not include your list of references)
- Responses need to be substantive by bringing information to the discussion or further enhance the discussion. Responses of “I agree” or “great post” does not count for the word count.
- Follow APA 7th edition
- Points will be deducted if the above is not followed
- Remember to use and follow APA-7th edition for all weekly assignments, discussion questions, and participation points.
- Here are some helpful links
- Student paper example
- Citing Sources
- The Writing Center is a great resource

