NURS 6512 Assignment Differential Diagnosis for Skin Conditions
Sample Answer for NURS 6512 Assignment Differential Diagnosis for Skin Conditions Included After Question
Properly identifying the cause and type of a patient’s skin condition involves a process of elimination known as differential diagnosis. Using this process, a health professional can take a given set of physical abnormalities, vital signs, health assessment findings, and patient descriptions of symptoms, and incrementally narrow them down until one diagnosis is determined as the most likely cause.
In this Lab Assignment, you will examine several visual representations of various skin conditions, describe your observations, and use the techniques of differential diagnosis to determine the most likely condition.
To Prepare
- Review the Skin Conditions document provided in this week’s Learning Resources, and select one condition to closely examine for this Lab Assignment.
- Consider the abnormal physical characteristics you observe in the graphic you selected. How would you describe the characteristics using clinical terminologies?
- Explore different conditions that could be the cause of the skin abnormalities in the graphics you selected.
- Consider which of the conditions is most likely to be the correct diagnosis, and why.
- Search the Walden library for one evidence-based practice, peer-reviewed article based on the skin condition you chose for this Lab Assignment.
- Review the Comprehensive SOAP Exemplar found in this week’s Learning Resources to guide you as you prepare your SOAP note.
- Download the SOAP Template found in this week’s Learning Resources, and use this template to complete this Lab Assignment.
The Lab Assignment
- Choose one skin condition graphic (identify by number in your Chief Complaint) to document your assignment in the SOAP (Subjective, Objective, Assessment, and Plan) note format rather than the traditional narrative style. Refer to Chapter 2 of the Sullivan text and the Comprehensive SOAP Template in this week’s Learning Resources for guidance. Remember that not all comprehensive SOAP data are included in every patient case.
- Use clinical terminologies to explain the physical characteristics featured in the graphic. Formulate a differential diagnosis of three to five possible conditions for the skin graphic that you chose. Determine which is most likely to be the correct diagnosis and explain your reasoning using at least three different references, one reference from current evidence-based literature from your search and two different references from this week’s Learning Resources.
By Day 7 of Week 4
Submit your Lab Assignment.
Submission and Grading Information
To submit your completed Assignment for review and grading, do the following:
- Please save your Assignment using the naming convention “WK4Assgn1+last name+first initial.(extension)” as the name.
- Click the Week 4 Assignment 1 Rubric to review the Grading Criteria for the Assignment.
- Click the Week 4 Assignment 1 link. You will also be able to “View Rubric” for grading criteria from this area.
- Next, from the Attach File area, click on the Browse My Computer button. Find the document you saved as “WK4Assgn1+last name+first initial.(extension)” and click Open.
- If applicable: From the Plagiarism Tools area, click the checkbox for I agree to submit my paper(s) to the Global Reference Database.
- Click on the Submit button to complete your submission.
A Sample Answer For the Assignment: NURS 6512 Assignment Differential Diagnosis for Skin Conditions
Title: NURS 6512 Assignment Differential Diagnosis for Skin Conditions
SUBJECTIVE DATA
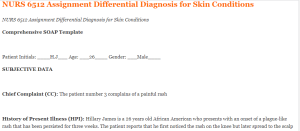
Chief Complaint (CC): The patient number 3 complains of a painful rash
History of Present Illness (HPI): Hillary James is a 26 years old African American who presents with an onset of a plague-like rash that has been persisted for three weeks. The patient reports that he first noticed the rash on the knee but later spread to the scalp and elbows. He indicates that the rash is itchy. The patient is disturbed by the condition and indicates that she has been stressed as the issue seems to progress. She has over-the-counter painkiller medication to help relieve the pain. He indicates that the rashes are severe and the associated pain to be 7/10. He suspects that he acquired the skin condition during camping three weeks ago.
Medications: The patient’s current medication includes ibuprofen 400mg PO every 8 hours.
Allergies: The patient has no known drug or food allergy.
Past Medical History (PMH): The patient was recently treated for recurring tonsillitis. He denies having been hospitalized for the past 12 months.
Past Surgical History (PSH): The patient has undergone any surgical procedure in his life.
Sexual/Reproductive History: The patient is married to one wife and they have three children.
Personal/Social History: The patient denies using tobacco or any illicit drug. On the other hand, he enjoys taking alcohol, especially on the weekends. Furthermore, he likes traveling and making new friends.
Immunization History: The patient’s immunization is up to date. His last Tdap was three years ago. Also, he received the flu vaccine a year ago. On the other hand, the patient was not eligible for the pneumonia vaccine at the time he came to the clinic.
Significant Family History: The patient denies a family history of dermatitis or skin rashes.
Lifestyle: The patient works as an electrical technician. He states that he goes to church every Sunday despite his drinking habits. Also, he sleeps late sometimes because of his demanding work. He has an insurance plan and so seeks medical interventions regularly whenever he feels unwell. Furthermore, the patient indicates that he participates in regular dieting and physical exercise. He believes that living an active life reduces the risks of cardiovascular diseases and other conditions.
Review of Systems:
General: The patient is alert and denies experiencing night sweats. He has not gained or lost weight in the past six months. The patient appears energetic; though, slightly disturbed by the skin lesion. Furthermore, the patient has no nail or hair change.
HEENT: There are no changes in the hearing or vision. The patient has a normal visual acuity. The head is intact with no injuries.
Neck: The neck is supple with a full range of motion. There are no signs of lymphadenopathy noted.
Breasts: n/a
Respiratory: No signs of dyspnea or murmurs from the lungs. The lungs are symmetrical. The patient has a normal heart rhythm.
Cardiovascular/Peripheral Vascular: The blood pressure is normal. No signs of peripheral edema.
Gastrointestinal: The patient has a normal bowel movement.
Genitourinary: No pain during micturition. The patient empties their bladder completely
Musculoskeletal: The patient has a full range of motion. No pain in the muscles indicated.
Psychiatric: The patient is calm and cooperative. No signs of depression or hallucination
Neurological:
Skin: Include rashes, lumps, sores, itching, dryness, changes, etc.
Hematologic: Normal C2-C12
Endocrine:
Allergic/Immunologic: NKDA
OBJECTIVE DATA: From head-to-toe, include what you see, hear, and feel when doing your physical exam. You only need to examine the systems that are pertinent to the CC, HPI, and History unless you are doing a total H&P. Do not use WNL or normal. You must describe what you see.
Physical Exam:
Vital signs: Ht 5’8’’ Wt=137 lbs, BMI=24.8, T=37.2 degrees Celsius, BP = 125/73mmhg
General: The patient is oriented and well-nourished.
HEENT:
Neck: No JVD
Chest/Lungs: The lung and chest are symmetrical and clear to auscultate
Heart/Peripheral Vascular: Normal heart rate, no cyanosis
Abdomen: Soft, non-tender, and non-distended.
Genital/Rectal:
Musculoskeletal: Full range of motion
Neurological: C2-C12 intact
Skin: the moist, presence of lesions and painful rashes. The pain increases in hot temperatures and on touch.
ASSESSMENT:
The differential diagnosis for the patient includes contact dermatitis, heat rash, and plaque psoriasis. Contact dermatitis is a condition characterized by causes reddening on the skin and mainly emerges when the skin comes to contact with chemicals (Esser & Martin, 2020). The main symptoms include dry skin and oozing blisters. Also, the patient may their skin turn dark, or swell. In this case, the patient skin is itchy and produces oozing blisters (Yadav, 2021).
The second diagnosis is heat rash, a condition resulting from the blockage of the sweat ducts. The signs and symptoms of heat rash include red bumps on the skin. The patient presents with rashes that are characterized by red bumps and some of them scaly.
The third diagnosis is plaque psoriasis, a condition characterized by raised red patches covered with white build-up (Havnaer & Han, 2019). The kin condition usually shows up in the knees and scalp. The common causes of plaque psoriasis include autoimmune diseases where the body’s immune system fights the healthy cells. Furthermore, injuries to the skin could also trigger the reaction (Rendon & Schäkel, 2019).
REFLECTION:
The clinical experiences provided a good opportunity for learning about the various skin conditions and their presentations. A clear analysis of the skin characteristics in terms of size, component, and the nature of swelling may help in making the right diagnosis. On the other hand, many skin conditions could assume similar characteristics and this makes them prone to misdiagnosis. Furthermore, it was apparent that skin conditions can be traumatizing especially when they are itchy. Patients tend to feel uncomfortable and so the treatment plan should focus on providing relevant psychological counseling to the victims (Wu et al., 2020).
Understanding the anatomical structures of the skin helps in identifying the affected areas and the possible contributing factors. Furthermore, hormonal changes in the body also cause a skin rash; therefore, the hallmark in the diagnosis and treatment process is to identify the causative factors and address them. Not all conditions may require medical intervention as some may only need skincare (Havnaer & Han, 2019). Furthermore, it was evident that having theoretical knowledge is important in the diagnosis process. However, the causes and manifestations of the skin conditions may vary from one individual to the other depending on the socio-cultural and demographic factors.
Besides, the clinical experience allowed me to take a patient’s history and interact with them to understand their underlying conditions and the possible contributing factors. Creating a conducive environment is necessary during the history taking to allow the patients to feel comfortable and share vital information that could help in better management of their conditions. The patient was cooperative and ready to share. He described the onset of the conditions and exposure factors that could be linked with it.
On the other hand, I felt like I did not provide adequate patient education to the client. Patient education is important in equipping the patient with self-care skills and addressing possible social and cultural factors that could be affecting their health condition. Proper hygiene is dietary intake is important. Therefore, in the subsequent clinical practice, I would consider taking good time to offer relevant patient education to improve the treatment outcomes. Other than the nutritional education, I will let the client understand the importance of identifying the skin irritants and avoiding them. Most of the patients tend to seek anti-allergy medications without confirming what illnesses they are having. Skin conditions, like any other disease, may have a poor prognosis if not treated in time.
I agree with the preceptor based on the evidence. The literature analyzed indicates the variations in the characteristics of the various skin conditions. However, there are key features used in the diagnosis that was relevant in this case and guided the differential diagnosis.
References
Esser, P. R., & Martin, S. F. (2020). Extended understanding of pathogenesis and treatment of contact allergy. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete, 71(3), 174-181. https://doi.org/10.1007/s00105-019-04527-9
Havnaer, A., & Han, G. (2019). Autoinflammatory disorders: a review and update on pathogenesis and treatment. American journal of clinical dermatology, 20(4), 539-564.
Rendon, A., & Schäkel, K. (2019). Psoriasis pathogenesis and treatment. International journal of molecular sciences, 20(6), 1475.
Wu, H., Yin, H., Chen, H., Sun, M., Liu, X., Yu, Y., Tang, Y., Long, H., Zhang, B., Zhang, J., Zhou, Y., Li, Y., Zhang, G., Zhang, P., Zhan, Y., Liao, J., Luo, S., Xiao, R., Su, Y., … Lu, Q. (2020). A deep learning, image-based approach for automated diagnosis for inflammatory skin diseases. Annals of Translational Medicine, 8(9), 581-581. https://doi.org/10.21037/atm.2020.04.39
Yadav, A. (2021). A study of diagnosis of skin disease using deep learning techniques. International Journal for Research in Applied Science and Engineering Technology, 9(3), 771-774. https://doi.org/10.22214/ijraset.2021.33310
Click here to ORDER an A++ paper from our MASTERS and DOCTORATE WRITERS: NURS 6512 Assignment Differential Diagnosis for Skin Conditions
A Sample Answer 2 For the Assignment: NURS 6512 Assignment Differential Diagnosis for Skin Conditions
Title: NURS 6512 Assignment Differential Diagnosis for Skin Conditions
SUBJECTIVE DATA: “I have indented reddened streaks on my skin that started appearing on the second month when I became pregnant.” “Too many stretch marks on my stomach since being pregnant”
Chief Complaint (CC): Picture #2- I have a concern with the stretch marks on my stomach which first noticed at the end of my first trimester in pregnancy.
History of Present Illness (HPI): Ms Caroline Fisher is a 32 year old female is a gravida 1, para 0 Black American who is pregnant and in her 24 weeks gestational period who came today and complained about the changes she has been noticing on her abdomen that is characterized by streaks of reddened skin which continued to darken as the pregnancy progresses, last menstrual period was 9/21/21. Ms Caroline stated that the stretchmarks are more prominent on the anterior abdominal while few lines run towards the back. Ms Caroline at this time stated that sometimes she feels itchy but denies any pain or any discomfort. Ms Caroline stated that her friends introduced her to an herbal therapy known as cocoa butter which she has been apply but no obvious changes. Ms Caroline is so much concerned about the recent changes to her body and skin and doesn’t feel good about her recent look, Ms Caroline has a believe that she has actually put on weight and that might have worsened the stretchmarks.
Medications:
Patient is on the following medications;
Pregnacare which contains mostly vitamins
400 μg of folic acid prescribed once daily
Iron 600mg Daily
Metformin 500mg twice daily for diabetes
Norvasc 10mg daily for hypertension
Allergies: Allergic to Sulphur medications. No known food allergies.
Past Medical History (PMH): Ms Craoline is a known Type 2 diabetic patient, was last hospitalized in 2020 prior to her recent pregnancy on account of uncontrolled hyperglycemia which was managed and well controlled during the 2 days’ hospitalization before being discharged, patient also has history of borderline hypertension.
Past Surgical History (PSH): Patient denies any surgical history.
Sexual/Reproductive History: Ms. Caroline is Straight and is sexually active. No positive history of sexual abuse, has had 2 partners since she became sexually active. Menarche started at the age of 12 and since then have always had a regular menstrual cycle of 28days.
Personal/Social History: Ms Caroline is an elementary school teacher and lives with the boyfriend in a single family house. Denied history of illegal drug use, drinks alcool occasionally but stopped since she got pregnant.
Health Maintenance: Ms Caroline has been compliant with her regular pregnancy checkup and consults as advised.
Immunization History: Mrs Coroline is upto date with her vaccinations including covid vaccine and the last immunization was the flu shot which she got on 1/3/22
Significant Family History: Father has history of Diabetes which is well controlled with insulin and Mother had hypertension before her death at the age of 60 years in 2021 due to complication of coronavirus.
Review of Systems:
General: Ms Caroline is in a stable condition, no obvious distress noted. She just doesn’t feel good about the recent skin changes since she got pregnancy as that is her first pregnancy.
HEENT: Ms. Caroline denies having any problems with hearing, vision, nasal congestions, nil swelling and no remarkable change on the throat.
Respiratory: Ms Caroline denies any breathing problems
Cardiovascular/Peripheral Vascular: Ms Caroline denies any episodes of irregular heartbeats, denies any heart murmur and not chest pain.
Gastrointestinal: Patient denies any problems with appetite. Confirmed she has regular bowel movements. Patient is positive for constipation occasionally.
Genitourinary: Patient denies any history of urinary tract infection.
Musculoskeletal: Patient is positive mild back pain which she takes regular Tylenol 375mg orally every 8 hrs. when needed.
Neurological: Patient is alert and oriented, no neurological deficit noted. Denies any history of epilepsy or seizures.
Psychiatric: Patient denies any history of mental health illness.
Skin/hair/nails: Ms Caroline is very much concerned about the new stretch
marks that runs through her abdominal wall. Patient does not have any other skin alteration. Patient complained of hair dandruff.
OBJECTIVE DATA:
Physical Exam:
Vital signs: Patients blood pressure measured on the right arm was 144/81, Temperature is 97.7 degree Fahrenheit, Pulse is 72bpm, Respiration is 17c/m, Weight is 179 pounds, height is 5 feet 6 inches and a calculated BMI of 28.9.
General: Ms. Caroline came in alert and oriented to time and place. The vital signs showed that the patient is overweight with a BMI of 28.9 and blood pressure is elevated.
HEENT: On examination of the hair, there were presence of dandruff on the scalp.No inflammation noted on the tonsil and no tenderness noted at the temporomandibular joint. The pupils were equal, round, reactive to light. No discharges noted from ears.
Neck: There was normal range of motion, and no distended juggler vein noted.
Chest/Lungs: The trunk was clear. The intercostal movements were nornmal.no abnormal breath sounds like wheezes. Respiration rate of 18 b/min.
Heart/Peripheral Vascular: On auscultation, the S1 and S2 heart sounds were present and heart rate was within normal limits of 72bpm.
Abdomen: There was positive fetal heart rate of about 128b/m and thee were marked indented streaks on the abdominal wall.
Genital/Rectal: The vagina was free from any signs of infection, nil swelling, discharge or inflammation noted during assessment of the genitalia.
Musculoskeletal: There are no muscle or joint pains noted and there is full range of motion with no limitation.
Neurological: Mrs Caroline is oriented to time, place and person. Patient scored high on assessment of mental status. The mental assessment shows patient has memory intact both recent and past events.
Skin: Patients skin is warm to touch with a temperature of 97.8, nil discoloration noted except the indented stretch marks on the abdominal wall
Diagnostic results:
- There was Lab draw for White blood count which was unremarkable for infection
- On observation of the skin, the streaks and discoloration of the skin were present
- A culture of the skin is important to rule other causes of skin infections.
- Scraping of the nail and skin is key to rule out infections of the skin (Colyar,2015).
ASSESSMENT:
Differential diagnoses
- Linea nigra
- Linear focal elastosis
- Striae from topical steroid abuse, such as in the treatment of psoriasis.
- Cushing’s syndrome.
Primary diagnosis:
After a thorough consideration of other possible causes of this condition, I was able to narrow down the diagnosis based on my assessments and patients present condition to be Striae gravid arum.
Pregnancy as we all know comes with different skin changes as the body adjust to the new normal of accommodating the baby such as the changes that occur within the connective tissues as the skin continues to stretch as the uterus enlarges leads to the stretch marks (Ball, J et.all 2019). This evidence of stretch march shows poor skin elasticity which further puts the patient at risk perineal or vaginal tears due to poor elasticity. When stretch marks becomes evident, it’s as a result of damage to the dermal collagen and further dilation of blood vessels (Dains, Baumann & Scheibel, 2019).
PLAN: This section is not required for the assignments in this course (NURS 6512) but will be required for future courses.
References
Colyar, M. R. (2015). Advanced practice nursing procedures. Philadelphia, PA: F. A. Davis.
Dains, J. E., Baumann, L. C., & Scheibel, P. (2019). Advanced health assessment and clinical diagnosis in primary care (6th ed.). St. Louis, MO: Elsevier Mosby.
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2019). Skin, hair, and nails: Student checklist. In Seidel’s guide to physical examination (9th ed.). St. Louis, MO: Elsevier Mosby.
Rubric Detail
Select Grid View or List View to change the rubric’s layout.
Content
Name: NURS_6512_Week_4_Assignment_1_Rubric
| Excellent | Good | Fair | Poor | ||
| Using the SOAP (Subjective, Objective, Assessment, and Plan) note format: · Create documentation, following SOAP format, of your assignment to choose one skin condition graphic (identify by number in your Chief Complaint). · Use clinical terminologies to explain the physical characteristics featured in the graphic. |
Points Range: 30 (30%) – 35 (35%)
The response clearly, accurately, and thoroughly follows the SOAP format to document one skin condition graphic and accurately identifies the graphic by number in the Chief Complaint. The response clearly and thoroughly explains all physical characteristics featured in the graphic using accurate terminologies. |
Points Range: 24 (24%) – 29 (29%)
The response accurately follows the SOAP format to document one skin condition graphic and accurately identifies the graphic by number in the Chief Complaint. The response explains most physical characteristics featured in the graphic using accurate terminologies. |
Points Range: 18 (18%) – 23 (23%)
The response follows the SOAP format, with vagueness and some inaccuracy in documenting one skin condition graphic, and accurately identifies the graphic by number in the Chief Complaint. The response explains some physical characteristics featured in the graphic using mostly accurate terminologies. |
Points Range: 0 (0%) – 17 (17%)
The response inaccurately follows the SOAP format or is missing documentation for one skin condition graphic and is missing or inaccurately identifies the graphic by number in the Chief Complaint. The response explains some or few physical characteristics featured in the graphic using terminologies with multiple inaccuracies. |
|
| · Formulate a different diagnosis of three to five possible considerations for the skin graphic. · Determine which is most likely to be the correct diagnosis, and explain your reasoning using at least three different references from current evidence-based literature. | Points Range: 45 (45%) – 50 (50%)
The response clearly, thoroughly, and accurately formulates a different diagnosis of five possible considerations for the skin graphic. The response determines the most likely correct diagnosis with reasoning that is explained clearly, accurately, and thoroughly using three or more different references from current evidence-based literature. |
Points Range: 39 (39%) – 44 (44%)
The response accurately formulates a different diagnosis of three to five possible considerations for the skin graphic. The response determines the most likely correct diagnosis with reasoning that is explained accurately using at least three different references from current evidence-based literature. |
Points Range: 33 (33%) – 38 (38%)
The response vaguely or with some inaccuracy formulates a different diagnosis of three possible considerations for the skin graphic. The response determines the most likely correct diagnosis with reasoning that is explained vaguely and with some inaccuracy using three different references from current evidence-based literature. |
Points Range: 0 (0%) – 32 (32%)
The response formulates inaccurately, incompletely, or is missing a different diagnosis of possible considerations for the skin graphic, with two or fewer possible considerations provided. The response vaguely, inaccurately, or incompletely determines the most likely correct diagnosis with reasoning that is missing or explained using two or fewer different references from current evidence-based literature. |
|
| Written Expression and Formatting – Paragraph Development and Organization: Paragraphs make clear points that support well-developed ideas, flow logically, and demonstrate continuity of ideas. Sentences are carefully focused–neither long and rambling nor short and lacking substance. A clear and comprehensive purpose statement and introduction are provided that delineate all required criteria. |
Points Range: 5 (5%) – 5 (5%)
Paragraphs and sentences follow writing standards for flow, continuity, and clarity. A clear and comprehensive purpose statement, introduction, and conclusion are provided that delineate all required criteria. |
Points Range: 4 (4%) – 4 (4%)
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 80% of the time. Purpose, introduction, and conclusion of the assignment are stated, yet are brief and not descriptive. |
Points Range: 3 (3%) – 3 (3%)
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 60%–79% of the time. Purpose, introduction, and conclusion of the assignment are vague or off topic. |
Points Range: 0 (0%) – 2 (2%)
Paragraphs and sentences follow writing standards for flow, continuity, and clarity < 60% of the time. No purpose statement, introduction, or conclusion were provided. |
|
| Written Expression and Formatting – English writing standards: Correct grammar, mechanics, and proper punctuation |
Points Range: 5 (5%) – 5 (5%)
Uses correct grammar, spelling, and punctuation with no errors. |
Points Range: 4 (4%) – 4 (4%)
Contains a few (1 or 2) grammar, spelling, and punctuation errors. |
Points Range: 3 (3%) – 3 (3%)
Contains several (3 or 4) grammar, spelling, and punctuation errors. |
Points Range: 0 (0%) – 2 (2%)
Contains many (≥ 5) grammar, spelling, and punctuation errors that interfere with the reader’s understanding. |
|
| Written Expression and Formatting – The paper follows correct APA format for title page, headings, font, spacing, margins, indentations, page numbers, running heads, parenthetical/in-text citations, and reference list. | Points Range: 5 (5%) – 5 (5%)
Uses correct APA format with no errors. |
Points Range: 4 (4%) – 4 (4%)
Contains a few (1 or 2) APA format errors. |
Points Range: 3 (3%) – 3 (3%)
Contains several (3 or 4) APA format errors. |
Points Range: 0 (0%) – 2 (2%)
Contains many (≥ 5) APA format errors. |
|
| Total Points: 100 | |||||
Something as small and simple as a mole or a discolored toenail can offer meaningful clues
about a patient’s health. Abnormalities in skin, hair, and nails can provide non-invasive external
clues to internal disorders or even prove to be disorders themselves. Being able to evaluate such
abnormalities of the skin, hair, and nails is a diagnostic benefit for any nurse conducting health
assessments.
This week, you will explore how to assess the skin, hair, and nails, as well as how to evaluate
abnormal skin findings.
Learning Objectives
Students will:
Apply assessment skills to diagnose skin conditions
Apply concepts, theories, and principles relating to health assessment techniques and
diagnoses for the skin, hair, and nails
Analyze dermatologic procedures to include skin biopsy, punch biopsy, suture insertion
and removal, nail removal, skin lesion removal
Lopes Write Policy
For assignments that need to be submitted to Lopes Write, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
I do not accept assignments that are two or more weeks late unless we have worked out an extension.
As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
Important information for writing discussion questions and participation
Welcome to class
Hello class and welcome to the class and I will be your instructor for this course. This is a -week course and requires a lot of time commitment, organization, and a high level of dedication. Please use the class syllabus to guide you through all the assignments required for the course. I have also attached the classroom policies to this announcement to know your expectations for this course. Please review this document carefully and ask me any questions if you do. You could email me at any time or send me a message via the “message” icon in halo if you need to contact me. I check my email regularly, so you should get a response within 24 hours. If you have not heard from me within 24 hours and need to contact me urgently, please send a follow up text to
I strongly encourage that you do not wait until the very last minute to complete your assignments. Your assignments in weeks 4 and 5 require early planning as you would need to present a teaching plan and interview a community health provider. I advise you look at the requirements for these assignments at the beginning of the course and plan accordingly. I have posted the YouTube link that explains all the class assignments in detail. It is required that you watch this 32-minute video as the assignments from week 3 through 5 require that you follow the instructions to the letter to succeed. Failure to complete these assignments according to instructions might lead to a zero. After watching the video, please schedule a one-on-one with me to discuss your topic for your project by the second week of class. Use this link to schedule a 15-minute session. Please, call me at the time of your appointment on my number. Please note that I will NOT call you.
Please, be advised I do NOT accept any assignments by email. If you are having technical issues with uploading an assignment, contact the technical department and inform me of the issue. If you have any issues that would prevent you from getting your assignments to me by the deadline, please inform me to request a possible extension. Note that working fulltime or overtime is no excuse for late assignments. There is a 5%-point deduction for every day your assignment is late. This only applies to approved extensions. Late assignments will not be accepted.
If you think you would be needing accommodations due to any reasons, please contact the appropriate department to request accommodations.
Plagiarism is highly prohibited. Please ensure you are citing your sources correctly using APA 7th edition. All assignments including discussion posts should be formatted in APA with the appropriate spacing, font, margin, and indents. Any papers not well formatted would be returned back to you, hence, I advise you review APA formatting style. I have attached a sample paper in APA format and will also post sample discussion responses in subsequent announcements.
Your initial discussion post should be a minimum of 200 words and response posts should be a minimum of 150 words. Be advised that I grade based on quality and not necessarily the number of words you post. A minimum of TWO references should be used for your initial post. For your response post, you do not need references as personal experiences would count as response posts. If you however cite anything from the literature for your response post, it is required that you cite your reference. You should include a minimum of THREE references for papers in this course. Please note that references should be no more than 5 years old except recommended as a resource for the class. Furthermore, for each discussion board question, you need ONE initial substantive response and TWO substantive responses to either your classmates or your instructor for a total of THREE responses. There are TWO discussion questions each week, hence, you need a total minimum of SIX discussion posts for each week. I usually post a discussion question each week. You could also respond to these as it would count towards your required SIX discussion posts for the week.
I understand this is a lot of information to cover in 5 weeks, however, the Bible says in Philippians 4:13 that we can do all things through Christ that strengthens us. Even in times like this, we are encouraged by God’s word that we have that ability in us to succeed with His strength. I pray that each and every one of you receives strength for this course and life generally as we navigate through this pandemic that is shaking our world today. Relax and enjoy the course!
Hi Class,
Please read through the following information on writing a Discussion question response and participation posts.
Contact me if you have any questions.
Important information on Writing a Discussion Question
- Your response needs to be a minimum of 150 words (not including your list of references)
- There needs to be at least TWO references with ONE being a peer reviewed professional journal article.
- Include in-text citations in your response
- Do not include quotes—instead summarize and paraphrase the information
- Follow APA-7th edition
- Points will be deducted if the above is not followed
Participation –replies to your classmates or instructor
- A minimum of 6 responses per week, on at least 3 days of the week.
- Each response needs at least ONE reference with citations—best if it is a peer reviewed journal article
- Each response needs to be at least 75 words in length (does not include your list of references)
- Responses need to be substantive by bringing information to the discussion or further enhance the discussion. Responses of “I agree” or “great post” does not count for the word count.
- Follow APA 7th edition
- Points will be deducted if the above is not followed
- Remember to use and follow APA-7th edition for all weekly assignments, discussion questions, and participation points.
- Here are some helpful links
- Student paper example
- Citing Sources
- The Writing Center is a great resource

